Ovulación como signo de salud
(Ovulation a sign of health™)
-Revisión Teen STAR-
Autores: Yanara A. Bernal, María Antonia Villablanca, Virginia de la Lastra, Natalia Poblete Ahumada.
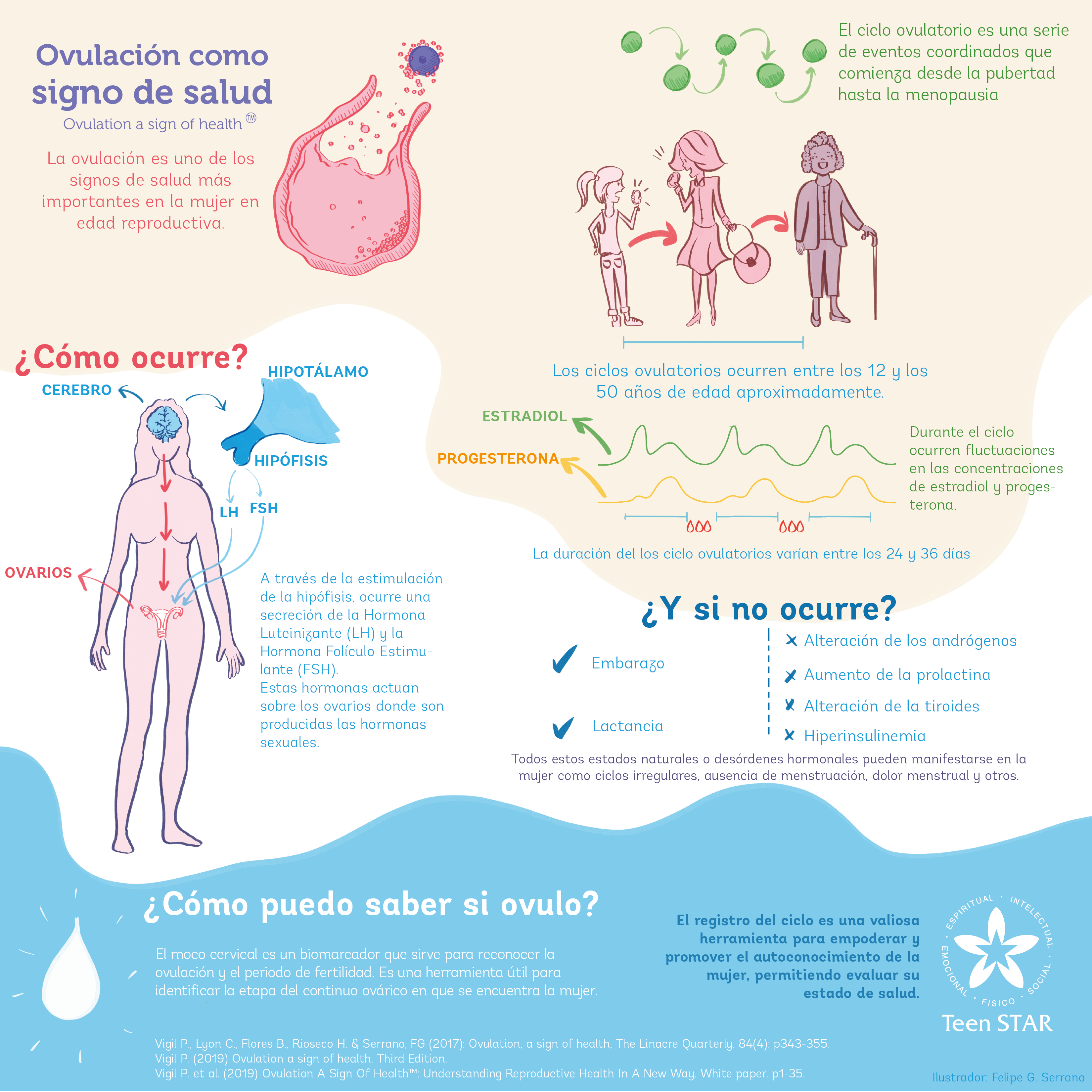
La ovulación es uno de los signos de salud más importantes en la mujer en edad reproductiva. Es un indicador que permite evaluar el estado hormonal y reproductivo de la mujer. Existen condiciones fisiológicas tales como el embarazo o lactancia, que producen un estado anovulatorio, es decir, sin ovulación, que es esperable dentro del continuo ovárico. También durante la pubertad y la perimenopausia, es esperable encontrar periodos de ovulación irregular ya que se consideran como períodos de transición. Sin embargo, fuera de estas situaciones normales, los estados en los cuales la ovulación ocurre de manera irregular, pueden ser un signo de condiciones de desequilibrio en la salud de la mujer. El estrés, alteraciones endocrinas, ginecológicas, genéticas, causas iatrogénicas o uso de medicamentos como anticonceptivos hormonales pueden alterar la ovulación, siendo muchas veces este el primer signo de un desorden hormonal. Sin embargo, a pesar de la gran importancia de este signo de salud, muchas mujeres desconocen su relevancia e impacto en su vida diaria. Conocer el significado de la ovulación permite corroborar el estado de salud de la mujer y, por tanto, detectar precozmente diversas patologías.
Para entender en profundidad por qué la ovulación es un signo de salud, en primer lugar es necesario conocer las principales estructuras anatómicas involucradas en el sistema reproductivo de la mujer. Los genitales internos son los ovarios, útero y oviductos o trompas uterinas (conocidas también, como trompas de Falopio). Los ovarios son responsables tanto de la producción de hormonas sexuales, estradiol y progesterona, como del desarrollo de los folículos. El folículo es una estructura que rodea a la célula germinal femenina, llamada ovocito. Según su etapa de desarrollo, el folículo se clasifica en: primordial, primario, secundario, terciario, maduro o de Graaf, cuerpo lúteo y albicans.
Una vez comprendida la anatomía, es necesario entender el rol del sistema nervioso central en la ovulación. El sistema nervioso central (SNC) es un conjunto de estructuras especializadas que controla diversas funciones, entre ellas la coordinación neuroendocrina del organismo. Las hormonas tienen un efecto crucial en el funcionamiento de distintas áreas del cerebro, incluyendo el hipotálamo y la hipófisis. La regulación del eje hipotálamo – hipófisis – gónada funciona mediante retroalimentación hormonal, es decir, el sistema responde a las concentraciones de una hormona, ya sea estimulando o suprimiendo la secreción hormonal. Además existen otras moléculas como la kisspeptina, que interviene en la regulación neuroendocrina, protagonista en el inicio de la pubertad.
En términos generales, a través de la estimulación de la hipófisis, se secreta la Hormona Luteinizante (LH) y Hormona Folículo Estimulante (FSH), ambas actúan en los ovarios para que éstos secreten hormonas sexuales.
Para comprender la ovulación también es necesario conocer el ciclo menstrual. Entre los 12 y los 50 años aproximadamente, es posible identificar ciclos ovulatorios. La duración de éstos varían entre 24 y 36 días. Durante el ciclo ocurren fluctuaciones en las concentraciones de estradiol y progesterona, lo que permite reconocer una fase folicular y lútea. La fase folicular, está caracterizada por un aumento del estradiol secretado por los folículos ováricos en crecimiento, esta fase dura desde el primer día de menstruación hasta la ovulación. Por otra parte la fase lútea corresponde al día después de la ovulación hasta el día anterior de la próxima menstruación. Por lo tanto, la duración del ciclo se determina contabilizando desde el primer día de menstruación hasta el día anterior a la próxima menstruación.
Las principales eventos de cada ciclo menstrual son: a) el crecimiento y desarrollo de un folículo ovárico y su ovocito, b) ovulación, c) crecimiento del endometrio uterino y d) desprendimiento del revestimiento endometrial (menstruación), en ausencia de fertilización.
Los eventos del ciclo menstrual comienzan con la elevación de los niveles de FSH, causando reclutamiento y desarrollo de los folículos terciarios, luego los folículos seleccionados, producen niveles crecientes de estradiol, frenando la secreción de FSH. El folículo dominante secreta altas concentraciones de estradiol, mientras que los demás se degeneran. Los altos niveles de estradiol genera una inducción de GnRH por parte de kisspeptina, provocando un peak de LH y posterior disminución de estradiol. El alza de LH inicia la luteinización del folículo ocasionando alza de progesterona en el periodo pre-ovulatorio, contribuyendo a la ruptura folicular favoreciendo la ovulación. El ovocito puede sobrevivir de 12 a 24 horas. La LH conduce a la formación y mantención del cuerpo lúteo. Éste produce progesterona y estradiol los cuales van aumentando hasta el 7º día después de la ovulación. Si la fertilización no ocurre, el cuerpo lúteo se comienza a degenerar disminuyendo los niveles de progesterona y estradiol. La vida media del cuerpo lúteo es entre 11 y 16 días. Cuando el cuerpo lúteo deja de producir las hormonas estradiol y progesterona, el endometrio (tejido que recubre la cavidad uterina) se descama y viene la menstruación. La baja de las hormonas estradiol y progesterona, permite el comienzo de un nuevo ciclo de reclutamiento folicular.
¿Cómo se puede reconocer la ovulación? Hay biomarcadores que permiten identificar la ovulación durante el ciclo menstrual. Reconocer la ovulación además de ser un signo de salud, permite a las mujeres y a las parejas que lo deseen identificar el día de mayor probabilidad de concepción. Además, con los signos que da la presencia o ausencia de moco cervical a la mujer a nivel de la vulva, se logra identificar la ventana de fertilidad.
De esta manera, una de las formas de lograr identificar el comienzo del periodo fértil es a través del reconocimiento de los cambios del moco cervical durante el ciclo. El moco cervical experimenta cambios a través del ciclo menstrual, debido a fluctuaciones de estradiol y progesterona, por lo tanto hay moco cervical estrogénico y progestativo.
El moco cervical estrogénico, es acuoso, transparente, fluido y cristalino, dando a la mujer una sensación húmeda y resbaladiza en la vulva. Durante este periodo, el moco cervical permite selección y ascenso de espermatozoides, por otro lado, la progesterona tiene un efecto contrario al estradiol en el cuello del útero, cambiando las características del moco cervical. El moco cervical progestagénico, es opaco y no fluido. El moco cervical es un biomarcador confiable para determinar la ovulación, el comienzo y fin de la fertilidad.
A través del registro del ciclo las mujeres pueden identificar la etapa del continuo ovárico en que se encuentran. Esto es de mucha utilidad tanto para la mujer como para los profesionales de la salud. Es una herramienta valiosa que fomenta el autoconocimiento de lo que ocurre en el ciclo mes a mes.
Los trastornos endocrinos que con mayor frecuencia producen alteraciones en la ovulación son i) trastornos en los andrógenos (como la testosterona) por ejemplo, el síndrome de ovario poliquístico, manifestándose en la mujer con: acné, presencia de vello excesivo, caída de cabello, aumento de peso y cambios de humor. ii) aumento en los niveles de prolactina originados por estrés, tumores hipofisarios y algunos medicamentos. En estos casos se observan fases lúteas cortas, anovulación, irregularidades menstruales, ausencia de menstruación (amenorrea), secreción de leche a través del pezón (galactorrea), sequedad de la piel, trastornos inmunológicos, baja líbido, sofocos y manos sudorosas; iii) trastornos tiroideos el hipotiroidismo conduce a menstruaciones irregulares, sangramiento abundantes (hipermenorrea y metrorragia) y sangrado inter-menstrual, además se asocia a síntomas depresivos, cansancio, letargo, aumento de peso, intolerancia al frío y pérdida de cabello; iv) aumento en los niveles de insulina, causada por resistencia a la insulina relacionada en algunos casos con la obesidad, aumento de peso, irregularidades menstruales y/o amenorrea.
Como ya se mencionó anteriormente, todos estos trastornos junto a otras alteraciones pueden manifestarse a través de cambios en el ciclo de la mujer, ya sea irregularidades menstruales, sangramiento abundante, ausencia de menstruación, dolor menstrual, entre otros.
La atención debe centrarse en la ovulación como signo de salud y como evento fundamental del ciclo de la mujer. Es la ovulación y no la menstruación el evento central en el ciclo en la mujer. Este concepto requiere de un cambio de paradigma, ya que hasta la fecha la atención en ocasiones se centra en la menstruación y no en la ovulación.
Lo anterior, rescata el valor del registro de ciclo como una herramienta para reconocer la ovulación y fomentar el autoconocimiento de la mujer, haciéndola partícipe junto a los profesionales de la salud en su bienestar.
Referencias
- Vigil P. et al. (2017). Ovulation, a sign of health. The Linacre Quarterly. 84(4): p343-355.
- Vigil P. (2019) Ovulation a sign of health. Third Edition.
- Vigil P. et al. (2019) Ovulation A Sign Of Health™: Understanding Reproductive Health In A New Way. White paper. p1-35.
Ovulation a sign of health™
-Teen STAR Review-
Authors: Yanara A. Bernal, María Antonia Villablanca, Virginia de la Lastra.
Ovulation is among the most trustworthy signs of health in women of reproductive age. It is an indicator that allows to assess the hormonal and reproductive status of women. There are physiological conditions such as pregnancy or lactation, which produce an anovulatory state. This means an absence of ovulation, which can be part of the ovarian continuum. During puberty and perimenopause, it is expected to find irregular ovulatory cycles, since these are considered as transition periods. However, outside these normal situations, irregular ovulatory or anovulatory cycles can be signs of an unhealthy lifestyle or illness. Stress, endocrine, gynecological and genetic disorders, iatrogenic causes or the use of medications as hormonal contraceptives, can disrupt ovulation, often being the first sign of a hormonal disorder. However, despite the importance of this sign of health, women are unaware of the relevance of their ovulation and the impact it has on their daily lives. If women knew the real meaning of this sign, they could detect a lot of health problems earlier.
A series of complex structures interact with each other in order to achieve ovulation. The ovaries, together with the uterus and oviducts (uterine tubes or Fallopian tubes), are part of the internal female genitals. The ovaries are responsible for the production of sex hormones, estradiol and progesterone, and the development of follicles. A follicle is a structure formed by the oocyte (the germinal cell) surrounded by somatic cells (granulosa cells). According to their developmental stage, follicles can be classified as primordial, primary, secondary, tertiary, mature (Graafian), corpus luteum and Albicans.
The central nervous system (CNS) is a specialized structure that controls the functions related to motor, behavioral, cognitive and neuroendocrine coordination of the body. Hormones have an important effect upon the wiring of different brain areas, including the hypothalamus and pituitary gland. The CNS is regulated by hormonal feedbacks. The main structures of the CNS involved in the regulation of ovulation are the hypothalamus and pituitary gland. Kisspeptin, a neuropeptide recently identified is synthesized by neurons located in the hypothalamus. These group of neurons, known as the kisspeptinergic system, have significant relevance in the onset of puberty. They induce the secretion of GnRH, stimulating the production of gonadotropic hormones: Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH). The gonadotropic hormones act upon the ovaries, where sex hormones are produced.
Women between 12 and 50 years of age normally exhibit regular ovulations characterized by 24 to 36 days cycles with fluctuating plasma estradiol and progesterone levels according to the different phases of the cycle. The first phase of the menstrual cycle is characterized by an increase in estradiol secretion by growing follicles. This phase starts with the first day of menstruation and lasts until ovulation. The luteal phase begins after ovulation and goes until the day before next menses. It is characterized by an increase in progesterone production by the corpus luteum.
The coordinated hormonal events required for ovulation are a) growth and development of an ovarian follicle and its oocyte, b) ovulation, c) preparation of the uterine lining (endometrium) to receive the zygote and d) endometrial lining detachment (menstruation), when fertilization does not occur.
At the beginning of each cycle, there is an increase in FSH levels that cause recruitment and development of antral follicles. FSH also triggers a progressive rise in estrogen production and secretion. After follicular recruitment, estradiol causes a decrease in FSH levels. A dominant follicle is selected, while the rest of the follicles degenerate. The dominant follicle produces increasingly higher levels of estradiol, which in turn stimulate kisspeptinergic neurons. Kisspeptin induces GnRH secretion and the pre-ovulatory LH peak, which initiates follicular luteinization leading to the formation of the corpus luteum. Before the initiation of the midcycle gonadotropin surge, a pre-ovulatory rise in progesterone occurs. This early progesterone rise produced by the pre-ovulatory follicle is critical for follicular rupture, a necessary process for ovulation. Progesterone maintains the LH peak causing follicular rupture, with the consequent release of the oocyte. The released oocyte will typically survive 12 to 24 hours. LH and progesterone contribute to the development and maintenance of the corpus luteum, which continues to produce progesterone and estrogen during the luteal phase. Normally this phase lasts for 11 to 16 days. If fertilization does not occur, the corpus luteum starts to regress. This regression causes a drop in estrogen and progesterone levels. The decrease in both hormones eliminates the suppression and a new cycle begins.
How to recognize ovulation?
Recognizing ovulation enables women and couples to identify the day when the probability of conception reaches its peak. With the signs given by the presence or absence of cervical mucus on the vulva, it is possible to identify the fertile window.
Cervical mucus undergoes several modifications during the phases of the reproductive cycle. Two main types of cervical mucus have been described: estrogenic and progestagenic. Increased estrogen levels halfway through the follicular phase result in a noticeable rise in the secretion of estrogenic mucus. The estrogenic cervical mucus is, transparent, fluid and crystalline, giving a slippery sensation in the vulva. During this period, cervical mucus allows sperm selection and ascent. Progesterone has the opposite effect of estradiol upon cervical mucus (antiestrogenic action). It inhibits production and changes the characteristics of the mucus to an opaque and less fluid mucus, with- out the ability to crystallize into palm leaf patterns.
The observation of changes in cervical mucus is considered a reliable biomarker as it has been demonstrated that recognizing mucus patterns can help women to identify the different stages of the ovarian continuum.
Endocrine abnormalities that can lead to ovulatory dysfunction are i) androgen disorders such as polycystic ovary syndrome, manifesting in women with acne, hirsutism, alopecia, increased body weight and mood changes; ii) increase in prolactin levels caused by stress, pituitary tumors, and some drugs. In these cases we can observe short luteal phases, anovulation, menstrual irregularities, amenorrhea, galactorrhea, skin dryness, immunological disorders, low libido, hot flashes, and sweaty hands; iii) thyroid disorders such as hypothyroidism which can lead to irregular menses, hypermenorrhea, metrorrhagia, and spotting, in addition to this, it is also associated with depressive symptoms, fatigue, lethargy, weight gain, cold intolerance and hair loss; iv) increase in insulin levels, caused by insulin resistance related in some occasion to obesity, weight gain, anovulation, menstrual irregularities, and amenorrhea.
All these disorders together with other alterations can manifest themselves through changes in woman’s cycles, either as menstrual irregularities, heavy bleeding, amenorrhea, menstrual pain, among others.
Often, healthcare providers have focused on regularizing bleeding patterns, without paying attention to ovulation in reproductive age women. Is important to consider ovulation as a sign of health and as the fundamental event of the women’s cycle.
For this reason, cycle charting is a valuable tool that empowers women, promoting self-knowledge and health care.
References
- Vigil P. et al. (2017): Ovulation, a sign of health. The Linacre Quarterly. 84(4): p343-355.
- Vigil P. (2019) Ovulation a sign of health. Third Edition.
- Vigil P. et al. (2019) Ovulation A Sign Of Health™: Understanding Reproductive Health In A New Way. White paper. p1-35.

Influence of sex steroid hormones on the adolescent brain and behavior: An update
Pilar Vigil, Juan Pablo del Río, Bárbara Carrera, Florencia C. Aránguiz,
Hernán Rioseco & Manuel E. Cortés
This review explains the main effects exerted by sex steroids and other hormones on the adolescent brain. During the transition from puberty to adolescence, these hormones participate in the organizational phenomena that structurally shape some brain circuits. In adulthood, this will propitiate some specific behavior as responses to the hormones now activating those neural circuits. Adolescence is, then, a critical “organizational window” for the brain to develop adequately, since steroid hormones perform important functions at this stage. For this reason, the adolescent years are very important for future behaviors in human beings. Changes that occur or fail to occur during adolescence will determine behaviors for the rest of one’s lifetime. Consequently, understanding the link between adolescent behavior and brain development as influenced by sex steroids and other hormones and compounds is very important in order to interpret various psycho-affective pathologies.
Lay Summary: The effect of steroid hormones on the development of the adolescent brain, and therefore, on adolescent behavior, is noticeable. This review presents their main activational and organizational effects. During the transition from puberty to adolescence, organizational phenomena triggered by steroids structurally affect the remodeling of brain circuits. Later in adulthood, these changes will be reflected in behavioral responses to such hormones. Adolescence can then be seen as a fundamental “organizational window” during which sex steroids and other hormones and compounds play relevant roles. The understanding of the relationship between adolescent behavior and the way hormones influence brain development help understand some psychological disorders.
Ovulation, a sign of health
Pilar Vigil, Carolina Lyon, Betsi Flores, Hernán Rioseco & Felipe Serrano
The concept of the ovarian continuum can be understood as a process that occurs during a woman’s lifetime and begins during intrauterine life with fertilization. Women start their reproductive years with approximately five hundred thousand follicles containing oocytes, of which only around five hundred will be released during ovulation. Ovulation has been recognized as an event linked with reproduction; however, recent evidence supports the role of ovulation as a sign of health. The use of biomarkers that help women recognize ovulation enables them to identify their health status. This knowledge helps medical healthcare providers in the prevention, diagnosis, and treatment of different pathologies related with endocrine disorders, gynecological abnormalities, autoimmune, genetic, and neoplastic diseases, as well as pregnancy-related issues. The knowledge of the ovarian continuum and the use of biomarkers to recognize ovulation should be considered a powerful tool for women and medical professionals.
Summary: The ovarian continuum is a process that occurs during a woman’s lifetime. It begins during intrauterine life with fertilization and ends with menopause. This process can be greatly affected by different conditions such as changes in hormonal levels and illnesses. Therefore, understanding and promoting the knowledge and use of biomarkers of ovulation in women is a key aspect to consider when evaluating their health status. The knowledge and education about the ovarian continuum should be taken into account as a powerful tool for women and medical professionals.
Steroid Hormones and Their Action in Women’s Brains: The Importance of Hormonal Balance
Juan Pablo Del Río, María I. Alliende, Natalia Molina, Felipe G. Serrano, Santiago Molina and Pilar Vigil
Sex hormones significantly impact women’s lives. Throughout the different stages of life, from menarche to menopause and all stages in between, women experience dramatic fluctuations in the levels of progesterone and estradiol, among other hormones. These fluctuations affect the body as a whole, including the central nervous system (CNS). In the CNS, sex hormones act via steroid receptors. They also have an effect on different neurotransmitters such as GABA, serotonin, dopamine, and glutamate. Additionally, studies show that sex hormones and their metabolites influence brain areas that regulate mood, behavior, and cognitive abilities. This review emphasizes the benefits a proper hormonal balance during the different stages of life has in the CNS. To achieve this goal, it is essential that hormone levels are evaluated considering a woman’s age and ovulatory status, so that a correct diagnosis and treatment can be made. Knowledge of steroid hormone activity in the brain will give women and health providers an important tool for improving their health and well-being.
The Importance of Fertility Awareness in the Assessment of a Woman’s Health a Review
Pilar Vigil, Leonard F. Blackwell, and Manuel E. Cortés.
Fertility awareness constitutes fundamental knowledge for every woman and is an important tool for health professionals. The objective of this review is to show how fertility awareness can be useful in the assessment of a woman’s health. The main techniques for detecting ovulation are explained, and then the events that characterize a normal menstrual cycle are discussed. The relevance of cervical mucus from the perspective of female fertility is highlighted. Finally, the usefulness of fertility awareness 1) to identify fertile and infertile periods, 2) to help to detect several pathologies, and 3) in regards to how it exerts an important role in the success of programs in education for affectivity and sexuality are discussed.